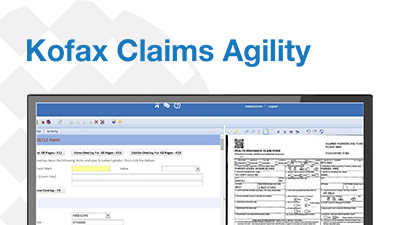
Optimize Health and Injury Claims Processing through Best Practice Medical Claims Automation
Processing and paying claims is the single largest operational cost for health, accident and injury insurers. Most claims processes are an inefficient combination of manual and digital steps spread over a variety of systems. Each manual step is a break in the workflow that not only causes delays, but also makes it nearly impossible to status each claim as it progresses, or know if bottlenecks have occurred or processing steps were skipped. Paper claims continue to drain resources, as these are inherently more costly to process than electronic claims, whether due to manual keying, use of antiquated OCR technology, or use of a third-party administrator.
Now you can take control of your claims process and handle more claims with fewer people and greater accuracy. Kofax Claims Agility™ automatically identifies the medical form type; captures, extracts and validates all data present on the forms; converts it to EDI; and routes it into your existing adjudication workstream, greatly improving the efficiency of your staff. As a result, your organization can replace existing manual workflows, or stop outsourcing claims processing and bring it in-house, providing greater control, process visibility and auditability over the entire process.
Drive Cost- and Process-Efficiencies by Digitizing Paper Claims
Capture all paper-based claims and transform the information into a time- and cost-saving digital format for automated processing and verification. Accurately extract and validate all subscriber, provider and medical information contained in service lines against medical code sets, NUBC, NUCC and EDI rules, insurer-specific rules, and master subscriber and provider data sources.
Streamline Workflows and Speed Claims Reimbursement
Optimize your claims processing workflow, enforce business controls, provide clear and actionable claims performance information and drive continuous process improvement. Staff may reject claims after reviewing identified errors, or claims may be auto-rejected via rules; examiners collaborate with billers through resolution, speeding the return and correction process. More importantly, only ‘clean claims’ are delivered to downstream processes, reducing adjudication exceptions and ensuring accurate payments.
Employ Best Practice Operational Analytics
Gain visibility of your claims processing performance and identify bottlenecks and cost-saving opportunities. The solution applies best practice workflows to every claim, so medical coding review and approval are efficient and conform to policy. Track and analyze throughput, operator performance and executed processes, and leverage this information to optimize processing and status claims and ensure compliance.













There are no reviews yet.